Sleepless Nights, Serious Risks: An Expert Guide to Reclaiming Deep Sleep & Optimal Health
TL;DR: Sleep Myths, Risks, and Solutions (Summary)
- Most adults need 7–9 hours of sleep: Short nights reduce immunity, heart health, metabolism, and mood.
- Alcohol, snoring, and weekend sleep-ins: All undermine deep, restorative sleep quality.
- Sleep hygiene basics: Fixed schedule, cool-dark-quiet bedroom, caffeine cut-off, morning sunlight, relaxing wind-down.
- CBT-I is the top non-drug fix: Cognitive Behavioral Therapy for Insomnia has an 80% success rate for persistent insomnia.
- Supplements: Only add melatonin, magnesium, valerian, or L-theanine after medical guidance.
- Prioritizing sleep: Improves nutrition, exercise, cognition, and longevity.
Many people might boast about pulling an all-nighter to meet a deadline or casually mention relying on a nightcap to drift off to sleep. These notions are common, but what if such widely held beliefs about sleep are not only incorrect but could also be actively undermining your sleep quality and overall well-being? For individuals dedicated to health—meticulously planning workouts, meals, and biohacking protocols—sleep hygiene tips often get overlooked. Yet restorative sleep isn't passive downtime; it's an active, essential biological process crucial for optimal health and the benefits of deep sleep¹. This guide will unveil the science behind sleep, debunk pervasive sleep myths, explore the profound risks of sleep deprivation, and empower you with evidence-based strategies and natural remedies for insomnia to achieve truly restorative rest. It's important to recognize that society sometimes glorifies "the hustle" at the expense of a consistent bedtime routine, potentially leading even the most health-conscious individuals to undervalue this critical pillar of well-being¹.
Putting Sleep Myths to Bed: The Scientific Truth
Understanding sleep begins with dismantling common misconceptions. These myths, often passed down or born from incomplete information, can lead to habits that unknowingly sabotage health. Addressing them with clear, evidence-based explanations can be both educational and empowering.
Myth 1: "I'm a Superhero! I Can Function Perfectly on Less Than 5 Hours of Sleep."
The notion that anyone can consistently thrive on minimal sleep is a pervasive—and dangerous—fallacy. While an extremely small fraction of people carry a rare genetic mutation allowing them to function on less rest, over 99 % of adults still need 7–9 hours of quality sleep per night to sustain optimal cognitive performance and overall health.
Believing you can "get by" on significantly less often springs from a subjective sense of coping that clashes with objective performance metrics. Sleep deprivation effects include impaired judgment and reduced self-awareness, making people poor judges of their own decline. This sets up a vicious cycle: insufficient sleep dulls judgment, leading someone to believe they're fine, which justifies further restriction and deeper impairment. Chronic sleep restriction—even when you feel functional—is linked to serious health risks of sleep deprivation, including diminished cognitive function and elevated odds of obesity, type 2 diabetes, heart disease, and high blood pressure⁵.
Myth 2: "A Glass of Wine (or a Beer) Before Bed Helps Me Sleep Like a Baby."
Sure, a nightcap can feel like the perfect way to drift off, but clinically it's a mirage. Alcohol is a mild sedative, so you'll nod off faster, yet it sabotages the very sleep architecture your brain relies on. Most patients don't realize that even a single drink chops up REM sleep—the phase that locks in memories, balances mood, and cements learning. A 2018 Sleep Medicine review showed alcohol can bump your risk of snoring and sleep apnea by roughly 25 percent.²
So yes, alcohol helps you fall asleep, but the sleep you get is light, fragmented, and anything but restorative. If you're knocking back a glass of wine to "help" you sleep and shrugging off the extra snoring as normal, you're quietly stacking the deck for daytime fog, poor recovery, and long-term cardiometabolic trouble. Swap the nightcap for a non-alcoholic tea or magnesium-rich snack, and you'll give your body the true deep-sleep edge it's been missing.
Myth 3: "Older People Just Don't Need as Much Sleep."
Yes, sleep patterns shift with age—your circadian rhythm may nudge you toward an earlier bedtime, and you might wake more often at night—but your baseline requirement doesn't shrink. Healthy adults over 60 still need roughly 7–9 hours of quality sleep to protect memory, immune strength, and metabolic health. The real culprits behind shortened nights in older adults are usually fragmented circadian signals, chronic pain, medications, or untreated conditions like restless-legs syndrome. Address those, and the sleep need remains the same.
Myth 4: "No Worries, I'll Catch Up on All My Lost Sleep Over the Weekend."
Think of sleep debt the way you think of credit-card interest: it accrues daily, and minimum payments (a Saturday sleep-in) barely dent the principal. One or two 10-hour mornings can soften the fatigue, but they don't repair the cognitive deficits—slower reaction time, poor focus—that build up after a week of 5-hour nights. Consistency is king. Keeping a stable sleep schedule—even on weekends—beats any "binge-sleep" strategy for long-term brain and heart health.
Myth 5: "Loud Snoring is Annoying, But It's Normal, Right?"
Occasional, soft snoring can be harmless. Chronic, window-rattling snoring is a red flag for obstructive sleep apnea (OSA), a disorder where your airway repeatedly collapses during the night. Untreated OSA drives up blood pressure, taxes the heart, raises the risk of stroke and type2 diabetes, and sabotages daytime focus. Watch for gasping, choking, or snorting sounds and daytime sleepiness¹. Not every snorer has sleep apnea, and not every apnea patient snores, but persistent loud snoring deserves a proper sleep study—your cardiovascular system will thank you.
Myth 6: "If I Can't Fall Asleep, I Should Just Stay in Bed and Force It."
If you've been tossing for twenty minutes, forcing it is the worst play. Staying in bed while wired teaches your brain that the mattress is a place for frustration, not rest. Instead, slip out of the bedroom, keep the lights low, and try a relaxing bedtime routine—light stretching, breath-work, or a few pages of a paperback. When genuine sleepiness returns, head back, and you'll cut sleep latency dramatically. Doing this rewires the "bed equals sleep" association and is one of the quickest tricks for how to fall asleep faster.¹ ⁹
The Unseen Toll: What Happens When Sleep is Insufficient?
Chronic sleep deprivation effects reach far beyond morning grogginess. Over time, too little shut-eye silently chips away at physical resilience, cognitive sharpness, and emotional stability—while boosting your accident risk. Prioritizing sleep isn't self-indulgent; it's non-negotiable preventive medicine.
A. Physical Health Under Siege: A Body Working Overtime
When the body doesn't get adequate sleep, several physiological systems begin to falter, leading to a cascade of negative health effects.
Weakened Immune Defenses
Deep sleep is when your body releases infection-fighting cytokines and antibodies. Skimping on rest drains those reserves, leaving you wide-open to every cold or flu bug in the room.⁴ ¹⁰
Cardiovascular Concerns
Five-hour nights raise high blood pressure, stiffen blood vessels, and spike stress hormones. Long-term studies link short sleep with higher odds of heart disease, heart attack, and stroke.¹³ ¹⁴ ⁷
Metabolic Disruption
Less sleep = more ghrelin (hunger) and less leptin (satiety). Result: late-night cravings, weight gain, and rising insulin resistance—all fast lanes toward type 2 diabetes and sluggish metabolism.¹¹ ¹⁰ ⁷
Silent Damage: Inflammation and vascular wear add up quietly, so people often fail to connect poor sleep today with major diagnoses tomorrow.¹⁰
B. The Brain in Crisis: Cognitive Fog and Emotional Turmoil
Sleep is indispensable for optimal brain function. When sleep is curtailed, cognitive abilities and emotional regulation suffer significantly.
Cognitive Impairment
Without adequate sleep, memory consolidation stalls, metabolic waste lingers in brain tissue, and reaction times slow. Even a single bad night tanks attention and problem-solving; chronic loss may literally cost neurons. Productivity, learning, and creativity nosedive.
Emotional Well-Being
Short sleep heightens irritability, anxiety, and depressive symptoms. Emotional regulation falters, relationships strain, and everyday stress feels bigger. In kids and teens, the same deficit shows up as impulsivity and mood swings.
C. Everyday Dangers: When Tiredness Turns Treacherous
Microsleeps—those split-second blackouts you don't feel coming—can strike at the wheel or on a job site. Research shows severe drowsy driving can be as impairing as (or worse than) a .08 BAC.¹³ ⁸ Because sleep-starved brains misjudge their own alertness, people often swear they're "fine"… right before a costly error.⁵
Remember, a weakened immune system means viruses hit harder, and groggy decision-making leads to comfort-food binges, multiplying downstream health risks.⁴
Strategies for Achieving Higher Quality Deep Sleep
Boosting sleep quality—especially the deep, restorative stages—takes a multi-pronged game plan. Foundational habits (what we call sleep hygiene) form your baseline, while targeted therapies such as Cognitive Behavioral Therapy for Insomnia (CBT-I) step in when habits alone don't cut it.
A. Foundational Habits: Mastering Sleep Hygiene – The Daily Toolkit for Better Nights
Sleep hygiene encompasses a range of daily practices and environmental adjustments designed to promote consistent, high-quality sleep. These habits are not just for those with diagnosed sleep problems; they represent proactive health maintenance that can optimize sleep for everyone. Consistent application is crucial for their effectiveness.
- Consistent Sleep Schedule: Go to bed and wake up at roughly the same time every day (yes, even weekends) to lock in a stable circadian rhythm.⁹
- Restful Sleep Sanctuary: Keep the bedroom cool (60–67 °F), dark, and quiet. Blackout curtains and white-noise machines are cheap upgrades.⁹
- Smart Caffeine & Alcohol Rules: Cut caffeine by 2 PM, skip nicotine at night, and trade the nightcap for herbal tea if you want genuine deep sleep.⁹
- Balanced Evenings: Finish heavy meals two hours before lights-out; going to bed stuffed (or starving) tanks sleep quality.⁹
- Daily Activity & Morning Sunlight: Regular exercise deepens slow-wave sleep; 30 minutes of early-day sunlight anchors your body clock.⁹ ¹⁸
- Nap with Intention: Power-nap 20–30 minutes before 3 PM or skip it—long, late naps rob nighttime sleep pressure.⁹
- Wind-Down Routine: Spend the last hour tech-free. Warm shower, breath-work, gentle stretches, or journaling tells your brain, "Sleep is next."¹
- Tame Racing Thoughts: Write tomorrow's to-do list before bed to clear mental clutter and fall asleep faster.¹
B. Evidence-Based Treatments for Persistent Sleep Issues: When Habits Aren't Enough
While good sleep hygiene is fundamental, some individuals may experience persistent sleep difficulties, such as insomnia, that require more targeted interventions.
1. Cognitive Behavioral Therapy for Insomnia (CBT-I): Retraining The Brain for Sleep:
CBT-I is a highly effective, evidence-based psychological therapy specifically designed to treat insomnia. It is often recommended as the first-line treatment, even before considering sleep medications. CBT-I focuses on identifying and changing the negative thoughts, unhelpful beliefs, and maladaptive behaviors that contribute to and perpetuate insomnia.
The therapy typically involves several components:
Sleep Education: Providing information about normal sleep patterns, the factors that influence sleep, and the mechanisms that maintain insomnia.
Behavioral Strategies: These include techniques like stimulus control, which aims to re-associate the bed and bedroom with sleep (e.g., only using the bed for sleep and intimacy, getting out of bed if unable to sleep within a certain timeframe), and sleep restriction, which temporarily limits time spent in bed to match actual sleep time, thereby increasing sleep drive and improving sleep efficiency.
Cognitive Restructuring: This involves identifying, challenging, and modifying dysfunctional thoughts and beliefs about sleep (e.g., "I'll never be able to function tomorrow if I don't get 8 hours of sleep") that can create anxiety and worsen insomnia.
Relaxation Training: Teaching various techniques to reduce physical and mental arousal, such as progressive muscle relaxation, diaphragmatic breathing, or mindfulness meditation.¹9
CBT-I is empowering because it equips individuals with long-term skills to manage their sleep, addressing the root causes of insomnia rather than just masking symptoms.20 Studies show that CBT-I can lead to significant improvements in sleep for up to 80% of people with insomnia, and many are able to reduce or discontinue sleep medications.¹9 The benefits are often durable and long-lasting.
2. When to Consult a Healthcare Professional: Don't Suffer in Silence
It is advisable to consult a healthcare professional if sleep problems are persistent, significantly impact daily functioning, or cause distress. Specific indicators include:
- Difficulty falling asleep, staying asleep, or waking too early on a regular basis.
- Experiencing significant daytime fatigue, irritability, or difficulty concentrating due to poor sleep.6
- Suspecting an underlying sleep disorder, such as sleep apnea (indicated by loud snoring, gasping, or pauses in breathing) or restless legs syndrome.
- Having other health conditions (e.g., chronic pain, depression, anxiety) that are either contributing to or being worsened by poor sleep.21 A doctor can help determine the cause of the sleep problem, which may involve a detailed sleep history, a physical examination, or referral for a sleep study (polysomnogram) if a sleep disorder is suspected.8 Treatment recommendations will be tailored to the individual's specific situation and may include lifestyle modifications, CBT-I, or, in some cases, medication.21
Exploring Supplements for Enhanced Deep Sleep: An Evidence-Based Look
Many individuals turn to dietary supplements in hopes of improving their sleep. While some supplements show promise, it's crucial to approach them with an understanding of the current scientific evidence, potential side effects, and interactions. The perception that "natural" equates to "safe" or "effective" is not always accurate, and the evidence for various sleep supplements varies considerably.
Crucial Disclaimer: Before considering any supplement, it is vital to discuss it with a healthcare provider. Supplements can have side effects and may interact with medications or underlying health conditions. The information provided here is for educational purposes only and is not a substitute for professional medical advice.22
A. Melatonin: The "Hormone of Darkness"
- Role & Evidence: Melatonin is a hormone naturally produced by the pineal gland in the brain, primarily at night, and plays a key role in regulating the body's sleep-wake cycle (circadian rhythm).22 Exogenous melatonin (taken as a supplement) has been studied for various sleep disorders. Evidence from systematic reviews and meta-analyses suggests it can be effective in reducing the time it takes to fall asleep (sleep onset latency) in individuals with primary insomnia and delayed sleep phase syndrome, and in helping to regulate sleep-wake patterns in blind individuals.24 One systematic review indicated that low-dose melatonin (0.3 mg or 1 mg) improved actual sleep time, sleep efficiency, and non-REM sleep (which includes deep sleep stages) in healthy, middle-aged volunteers.24 However, overall recommendations for melatonin use by healthy adults to optimize sleep are generally considered weak due to limited high-quality evidence and heterogeneity in studies.24 Healthcare providers often emphasize that melatonin is primarily a circadian rhythm regulator, not a potent sleep-inducing agent for everyone.26
- Dosage & Considerations: The amount of melatonin in over-the-counter products can vary widely, and quality control can be an issue.22 Higher doses are not necessarily more effective and may increase the likelihood of side effects or cause daytime drowsiness.26 Doses are typically 5 mg or less.26
- Side Effects & Interactions: Common side effects include headache, dizziness, nausea, and daytime drowsiness.22 Less common effects can include vivid dreams, short-term feelings of depression, and irritability.22 Melatonin can interact with various medications, including blood thinners (anticoagulants), anti-seizure medications, birth control pills, blood pressure medications, diabetes medications, and immunosuppressants.22
B. Magnesium: The Calming Mineral (with a spotlight on Magnesium L-Threonate)
- Role & Evidence: Magnesium is an essential mineral involved in hundreds of biochemical reactions in the body. Its potential role in sleep regulation may involve modulating neurotransmitter activity (such as enhancing GABA, an inhibitory neurotransmitter), inhibiting N-methyl-D-aspartate (NMDA) receptors (which can promote muscle relaxation), influencing melatonin production, and reducing levels of the stress hormone cortisol.27 A longitudinal study involving nearly 4,000 adults found that higher dietary magnesium intake was associated with better self-reported sleep quality and a lower likelihood of short sleep duration (<7 hours), particularly in individuals without depressive symptoms.27 More recently, a specific form, Magnesium L-Threonate (MgT), has garnered attention. A randomized controlled trial published in 2024 found that supplementation with 1 gram of MgT per day for 21 days significantly improved objectively measured deep sleep scores and REM sleep scores in adults aged 35-55 with self-reported sleep problems, compared to a placebo.28 Participants taking MgT also reported improvements in mood, energy, and daytime productivity.28
- Dosage & Considerations: The Recommended Dietary Allowance (RDA) for magnesium varies by age and sex. The MgT study used 1 gram per day.28 For general sleep improvement using other forms of magnesium, optimal dosages are not well-established from the provided information.
- Side Effects & Interactions: Common side effects of magnesium supplementation, particularly at higher doses or with certain forms like magnesium oxide, can include diarrhea, nausea, and abdominal cramping.29 Taking too much magnesium can lead to hypermagnesemia, with symptoms like flushing, hypotension, and impaired reflexes, although this is rare with normal kidney function.29 Magnesium supplements are generally contraindicated in individuals with renal failure due to the risk of accumulation.29 The MgT study reported that this specific form was safe and well-tolerated.28
C. Valerian Root: The Traditional Sleep Herb
- Role & Evidence: Valerian root (Valeriana officinalis) is an herb that has been traditionally used for centuries to treat insomnia and anxiety. Scientific evidence for its effectiveness is mixed. A systematic review of randomized controlled trials suggested that valerian might improve sleep quality, with individuals taking valerian being approximately 80% more likely to report improved sleep compared to those taking a placebo.31 However, this review also noted significant methodological problems in many of the included studies and evidence of publication bias (meaning studies with negative results might be less likely to be published).31 Furthermore, there was no consistent evidence from polysomnography (objective sleep measurement) to show an impact on specific sleep stages like deep sleep.31 Another review suggested that inconsistent outcomes could be due to variable quality of herbal extracts and that whole root/rhizome preparations might be more reliable.32
- Dosage & Considerations: Dosages of valerian extract varied considerably in research studies, typically ranging from 225 mg to 1215 mg per day.31 Standardization of valerian preparations (e.g., to valerenic acid content) is not consistent across products, which can affect potency and outcomes.
- Side Effects & Interactions: While some sources suggest valerian is generally safe for short-term use 32, other reputable sources like Memorial Sloan Kettering Cancer Center (MSKCC) list potential side effects including daytime drowsiness, dizziness, headache, and, rarely, liver toxicity.33 MSKCC also provides significant warnings: valerian should be discontinued at least one week before surgery due to potential interactions with anesthesia. It should not be taken concurrently with barbiturates, benzodiazepines, other central nervous system depressants, or haloperidol. Individuals with pancreatic, liver, or gallbladder disease, or those who are pregnant or nursing, should avoid valerian. Due to its sedative effects, individuals should not drive or operate machinery after taking valerian.33
D. L-Theanine: The Calming Amino Acid from Tea
- Role & Evidence: L-theanine is an amino acid found primarily in green and black tea leaves and some mushrooms. It is known for its calming and anti-anxiety effects, thought to be mediated by its ability to increase levels of neurotransmitters like GABA, serotonin, and dopamine in the brain.35 While direct human trial evidence for L-theanine as a standalone sleep aid is less robust compared to melatonin or magnesium for certain conditions 37, some research is emerging. An animal study found that a mixture of GABA and L-theanine synergistically decreased sleep latency and improved both NREM (deep) sleep and REM sleep in mice.35 One review mentioned a study where L-theanine supplementation enhanced sleep quality, reduced sleep latency, and decreased sleep disturbances in humans.37 It is often used to promote relaxation without significant drowsiness.
- Dosage & Considerations: For promoting relaxation or sleep, L-theanine is often taken in the evening. Typical dosages range from 200 mg to 500 mg per day for most healthy adults, with a general recommendation not to exceed 500 mg daily.36 It can be taken with melatonin but should be used cautiously with other sedating medications.36
- Side Effects & Interactions: L-theanine is generally considered safe and well-tolerated for most people when taken at appropriate doses.36 Potential side effects, particularly at higher doses, may include headaches, dizziness, or mild gastrointestinal upset such as nausea.36 As with all supplements, the FDA classifies L-theanine as "generally recognized as safe" (GRAS) but does not regulate it as a drug, so product quality can vary.36
Sleep Supplement Snapshot: A Quick Guide
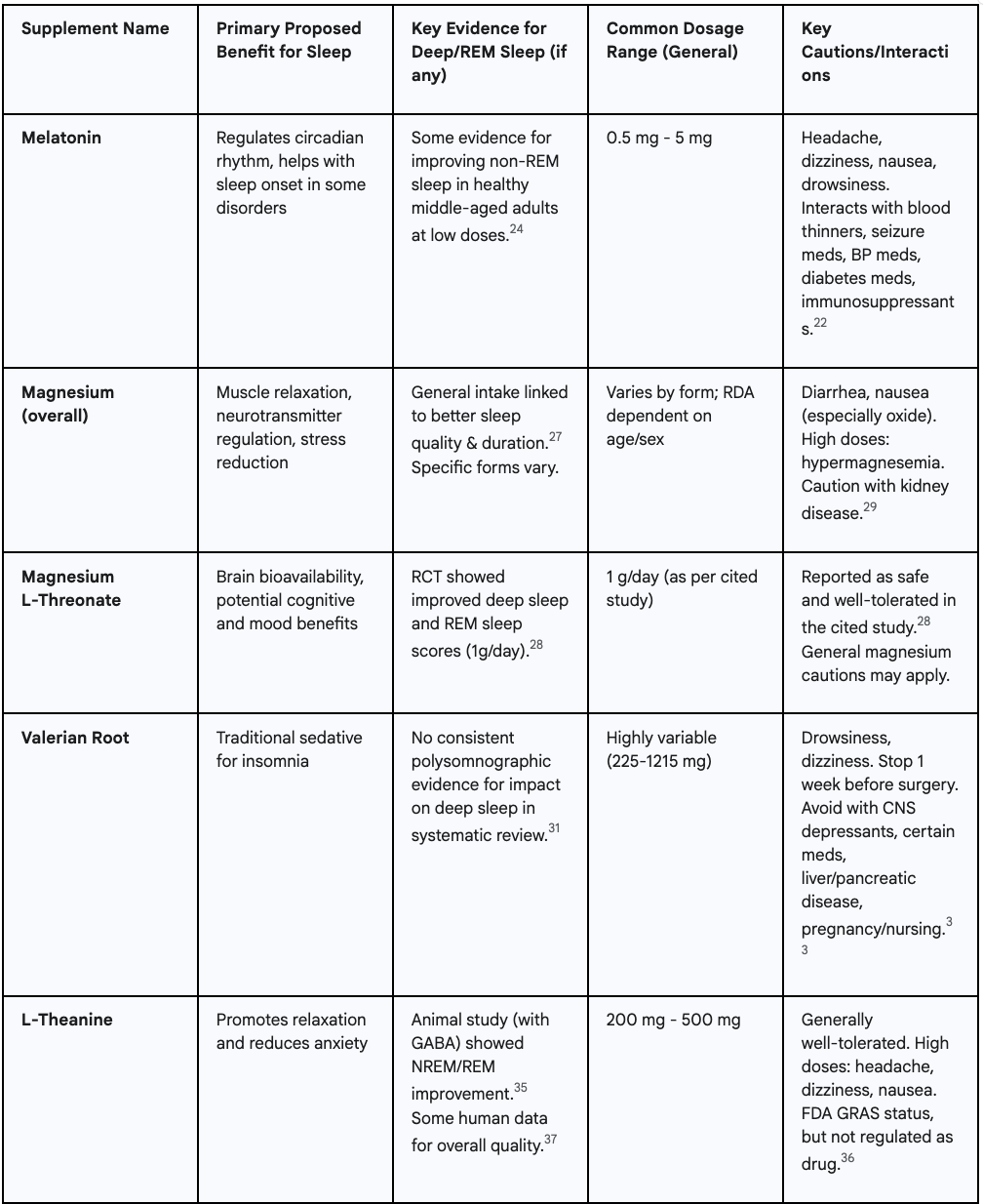
Individual responses to supplements can vary significantly due to factors like genetics, underlying health conditions, and the specific cause of sleep disturbance. This variability underscores why a one-size-fits-all recommendation is not feasible and why consultation with a healthcare professional is paramount before starting any new supplement regimen.
Conclusion: Prioritize Sleep, Transform Health – The Journey to Restorative Nights Starts Now
The evidence is unequivocal: sleep is not a passive luxury but a fundamental biological necessity, profoundly shaping every facet of physical health, mental clarity, and emotional stability. Quality sleep, especially the deep, restorative stages, powers the body's nightly repair, regeneration, and hormone balance. For health-conscious individuals, putting sleep on par with nutrition and exercise is non-negotiable; in fact, optimal sleep amplifies the gains you reap from clean eating and consistent workouts.
Armed with science that dismantles pervasive sleep myths and lays bare the genuine risks of sleep deprivation, you now hold the levers to transform sleep—and, by extension, overall health. The journey begins with conscious choices and consistent effort.
Start small: lock in one or two sleep hygiene practices this week—say, a fixed bedtime or a darker, cooler bedroom. If myth-driven habits have sabotaged rest, make an informed pivot. And if persistent sleep trouble shadows your days, book time with a healthcare professional to uncover root causes and explore solutions like CBT-I or targeted sleep studies.
Remember, investing in sleep is a direct investment in vitality, productivity, cognitive sharpness, emotional resilience, and long-term health. Sweet dreams are more than a pleasantry; they're the cornerstone of a vibrant, healthy life. Take the first step toward reclaiming restorative deep sleep tonight, and watch every other pillar of well-being rise with it.
Frequently Asked Questions (FAQ)
How many hours of sleep do adults really need for optimal health?
Most healthy adults thrive on 7–9 hours of quality sleep per night for peak cognition, immunity, and metabolic balance.
Can I catch up on sleep debt over the weekend?
No. Extra weekend sleep only partially repays sleep debt. Consistent nightly rest is the proven way to restore cognitive performance and hormone balance.
Does alcohol help or hurt sleep quality?
Alcohol may speed sleep onset but fragments REM sleep, raises snoring risk by 25%, and leaves you less rested.
Is loud snoring normal?
Persistent, loud snoring is a warning sign of obstructive sleep apnea and warrants a professional sleep study.
What is sleep hygiene and why does it matter?
Sleep hygiene means daily habits (consistent schedule, cool-dark room, caffeine cutoff) that reinforce your circadian rhythm and boost deep sleep.
Best first-line treatment for chronic insomnia?
Cognitive Behavioral Therapy for Insomnia (CBT-I) is a 6-to-8-week program that retrains thoughts and behaviors, effective for about 80% of sufferers.
Which supplements have evidence for better deep sleep?
Low-dose melatonin (0.5–5 mg), magnesium L-threonate (1 g), valerian root, and L-theanine show research promise but should be doctor-approved.
How long before bed should I stop caffeine?
Cut caffeine at least 6 hours before bedtime to prevent delayed sleep onset and lighter sleep stages.
Does exercise improve sleep quality?
Yes. Regular daytime exercise increases slow-wave (deep) sleep; avoid intense workouts within 2 hours of bedtime.
When should I see a doctor about sleep problems?
Seek help if you can't fall or stay asleep 3 or more nights per week for 3 months, feel daytime fatigue, or suspect sleep apnea.
Works cited
- Common Sleep Myths, Debunked by a Sleep Doctor, accessed May 7, 2025, https://sleepdoctor.com/how-sleep-works/sleep-myths
- Debunking Common Sleep Myths: Separating Fact from Fiction - Riverside Healthcare, accessed May 7, 2025, https://www.riversidehealthcare.org/blog/debunking-common-sleep-myths-separating-fact-fiction
- 8 common sleep myths debunked | Live Science, accessed May 7, 2025, https://www.livescience.com/common-sleep-myths-debunked
- Lack of sleep: Can it make you sick? - Mayo Clinic, accessed May 7, 2025, https://www.mayoclinic.org/diseases-conditions/insomnia/expert-answers/lack-of-sleep/faq-20057757
- Sleep deprivation - Wikipedia, accessed May 7, 2025, https://en.wikipedia.org/wiki/Sleep_deprivation
- Insomnia - Symptoms and causes - Mayo Clinic, accessed May 7, 2025, https://www.mayoclinic.org/diseases-conditions/insomnia/symptoms-causes/syc-20355167
- Debunked! 7 Common Sleep Apnea Myths and the Truth Behind Them | NuCara, accessed May 7, 2025, https://cpap.nucara.com/blog/post/debunked-7-common-sleep-apnea-myths-and-the-truth-behind-them
- Healthy Sleep - MedlinePlus, accessed May 7, 2025, https://medlineplus.gov/healthysleep.html
- Sleep tips: 6 steps to better sleep - Mayo Clinic, accessed May 7, 2025, https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/sleep/art-20048379
- Sleep Deprivation: Symptoms, Treatment, & Effects, accessed May 7, 2025, https://www.sleepfoundation.org/sleep-deprivation
- Sleep deprivation: Causes, symptoms, and treatment - Medical News Today, accessed May 7, 2025, https://www.medicalnewstoday.com/articles/307334
- Sleep | Chronic Disease Indicators - CDC, accessed May 7, 2025, https://www.cdc.gov/cdi/indicator-definitions/sleep.html
- Sleep Deprivation and Deficiency - How Sleep Affects Your Health ..., accessed May 7, 2025, https://www.nhlbi.nih.gov/health/sleep-deprivation/health-effects
- Mayo Clinic Q and A: Lack of sleep and risk of high blood pressure, accessed May 7, 2025, https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-q-and-a-lack-of-sleep-and-risk-of-high-blood-pressure/
- Mayo Clinic Minute: Lack of sleep worsens health issues - YouTube, accessed May 7, 2025, https://www.youtube.com/watch?v=UYPez6V_S54&pp=0gcJCfcAhR29_xXO
- Mental Health & Sleep | Sleep Health Foundation, accessed May 7, 2025, https://www.sleephealthfoundation.org.au/sleep-topics/mental-health-sleep
- Module 3. Functioning (Continued) Sleep deprivation impairs | NIOSH - CDC, accessed May 7, 2025, https://www.cdc.gov/niosh/work-hour-training-for-nurses/longhours/mod3/06.html
- National Sleep Foundation, accessed May 7, 2025, https://www.thensf.org/
- Cognitive Behavioural Therapy for Insomnia (CBT-I) | Sleep Health ..., accessed May 7, 2025, https://www.sleephealthfoundation.org.au/sleep-disorders/cognitive-behavioural-therapy-for-insomnia-cbt-i
- How Effective is CBT-I for Treating Insomnia? - The Insomnia and Sleep Institute of Arizona, accessed May 7, 2025, https://sleeplessinarizona.com/how-effective-is-cbt-i-for-treating-insomnia/
- Insomnia: Symptoms, Causes, Diagnosis, and Treatment - SleepApnea.org, accessed May 7, 2025, https://www.sleepapnea.org/insomnia/
- Melatonin side effects: What are the risks? - Mayo Clinic, accessed May 7, 2025, https://www.mayoclinic.org/healthy-lifestyle/adult-health/expert-answers/melatonin-side-effects/faq-20057874
- Sleeping Pills: How They Work, Side Effects, Risks & Types - Cleveland Clinic, accessed May 7, 2025, https://my.clevelandclinic.org/health/treatments/15308-sleeping-pills
- The effectiveness of melatonin for promoting healthy sleep: a rapid ..., accessed May 7, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4273450/
- Evidence for the efficacy of melatonin in the treatment of primary ..., accessed May 7, 2025, https://pubmed.ncbi.nlm.nih.gov/28648359/
- Mayo Clinic Minute: What to consider before using melatonin supplements for sleep, accessed May 7, 2025, https://www.youtube.com/watch?v=LLMc1qZGcd8
- Association of magnesium intake with sleep duration and sleep ..., accessed May 7, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8996025/
- Magnesium-L-threonate improves sleep quality and daytime ..., accessed May 7, 2025, https://pubmed.ncbi.nlm.nih.gov/39252819/
- Magnesium - StatPearls - NCBI Bookshelf, accessed May 7, 2025, https://www.ncbi.nlm.nih.gov/books/NBK519036/
- Magnesium Oxide: MedlinePlus Drug Information, accessed May 7, 2025, https://medlineplus.gov/druginfo/meds/a601074.html
- Valerian for Sleep: A Systematic Review and Meta-Analysis - PMC, accessed May 7, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4394901/
- Valerian Root in Treating Sleep Problems and Associated Disorders—A Systematic Review and Meta-Analysis - PubMed Central, accessed May 7, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7585905/
- Valerian | Memorial Sloan Kettering Cancer Center, accessed May 7, 2025, https://www.mskcc.org/pdf/cancer-care/patient-education/herbs/valerian
- Valerian | Memorial Sloan Kettering Cancer Center, accessed May 7, 2025, https://www.mskcc.org/cancer-care/integrative-medicine/herbs/valerian
- GABA and l-theanine mixture decreases sleep latency and improves ..., accessed May 7, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC6366437/
- L-Theanine: What It Is and 3 Benefits - Health Cleveland Clinic, accessed May 7, 2025, https://health.clevelandclinic.org/l-theanine
- Current Evidence on Common Dietary Supplements for Sleep Quality - PMC, accessed May 7, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11082867/

